Immunomodulatory and healing effects of Pranlukast (PRK) underlie its antitubercular efficacy
In a new study, researchers at IISc, led by Avadhesha Surolia and Raju S Rajmani from the Molecular Biophysics Unit (MBU), propose that induction of pranlukast (PRK) in anti-tubercular therapeutics augurs well for efficacious healing of lung tissues by recruiting pro-healing immune regulatory macrophages in TB-infected lungs. This, in turn, helps in improving efficacy and shortening the duration of the currently used TB treatment regimen.
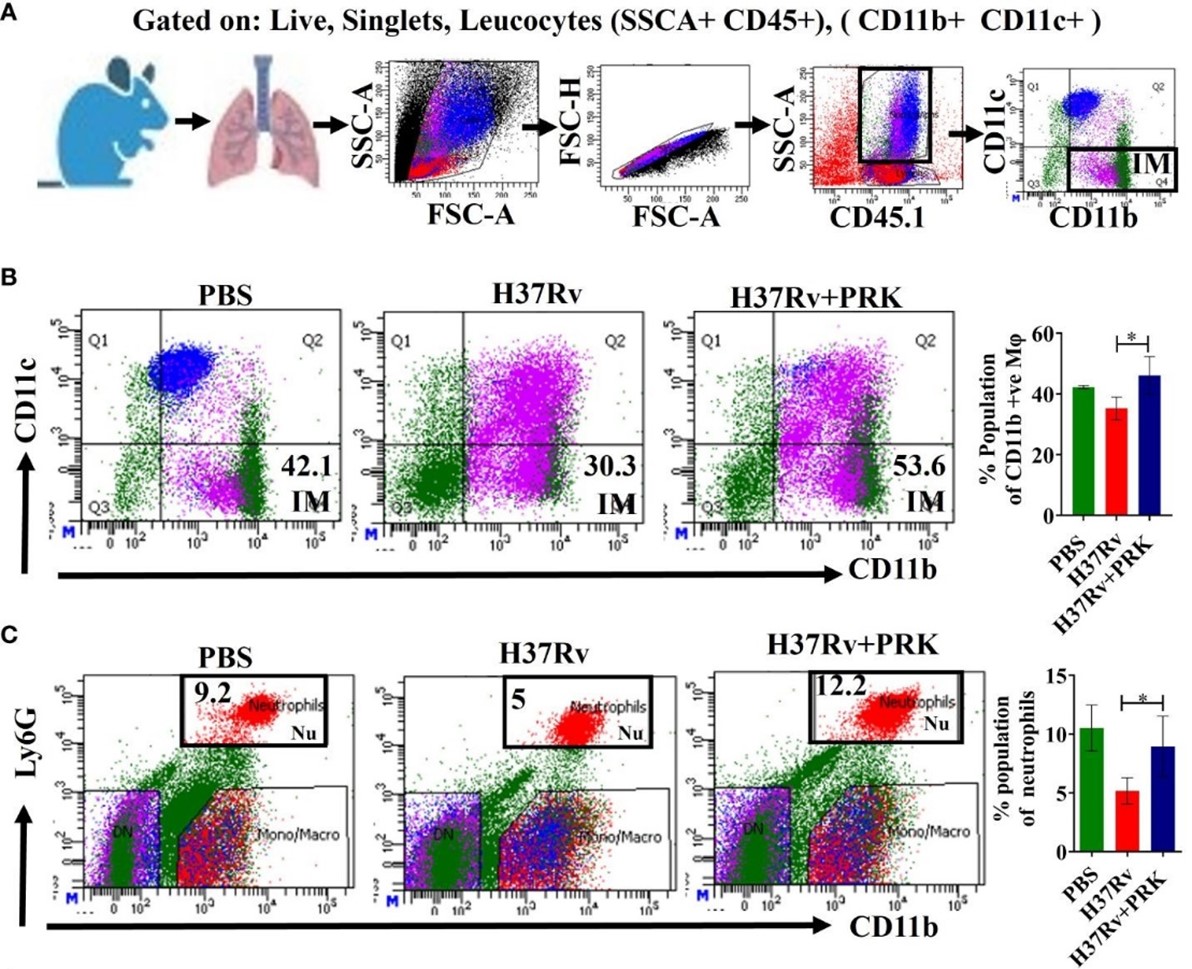
An understanding of the interactions and dynamics of the relationships between Mycobacterium tuberculosis (Mtb) and macrophages during the disease is essential to the design of host-directed, immunomodulation-dependent therapeutics to control tuberculosis. The two primary subtypes of macrophages found in the lungs are interstitial macrophages (IMs), which are generated from monocytes, and tissue-resident alveolar macrophages (AMs). AMs are an M2-type population that has anti-inflammatory qualities that help create a conducive atmosphere for the growth and virulence of Mtb. IMs, on the other hand, are linked to an immunological milieu that is more antibacterial.
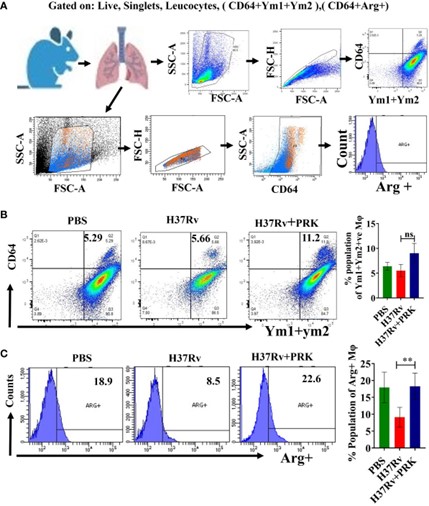
In the study, the team found that PRK reduced the bacterial burden in the lungs by decreasing the number of Mtb-susceptible alveolar macrophages (AMs) and increasing the population of pro-inflammatory interstitial macrophages (IMs). They also observed that PRK therapy increased the population of arginase 1 (Arg-1) and Ym1+Ym2 (chitinase 3-like 3) positive macrophages, which in turn promoted tissue healing and inflammation resolution.
In summary, these studies highlight that the induction of PRK in anti-tubercular therapies holds enormous value since it not only increases tissue repair but also reduces the tubercular load.
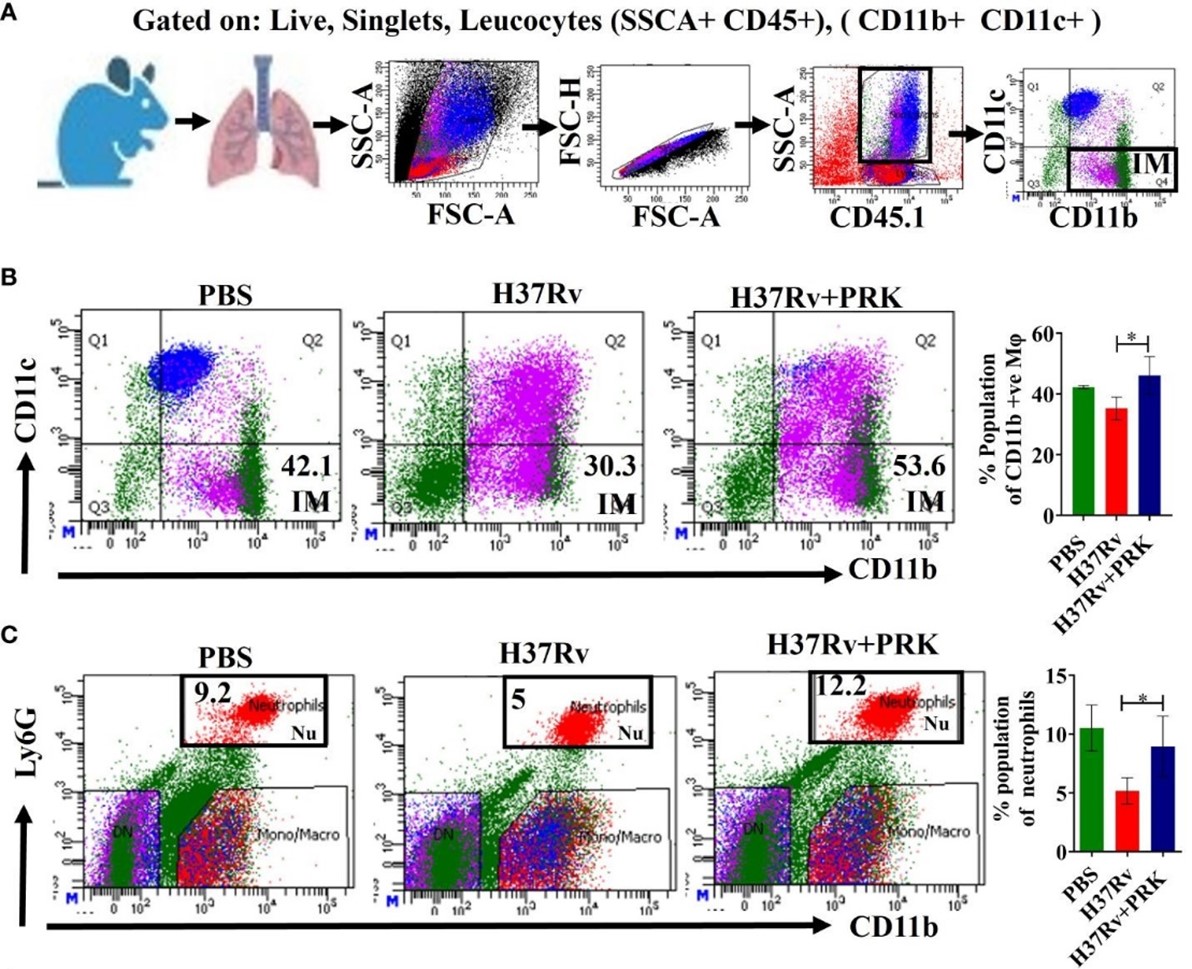
PRK therapy increased the population of CD11b+ (IMs) and CD11b+Ly6G+ (neutrophils) which in turn reduced the bacterial burden in the lungs
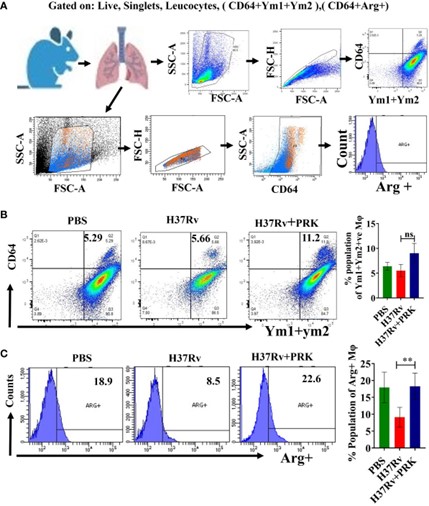
PRK therapy increased the population of arginase 1 (Arg-1) and Ym1+Ym2 (chitinase 3-like 3) positive macrophages, which in turn promoted tissue healing and inflammation resolution in the lungs of TB-infected mice
REFERENCE:
Rajmani RS, Surolia A, Antimycobacterial and healing effects of Pranlukast against MTB infection and pathogenesis in a preclinical mouse model of tuberculosis, Frontiers in Immunology (2024).
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1347045/full
LAB WEBSITE:
http://mbu.iisc.ac.in/aslab/public_html/index.html~